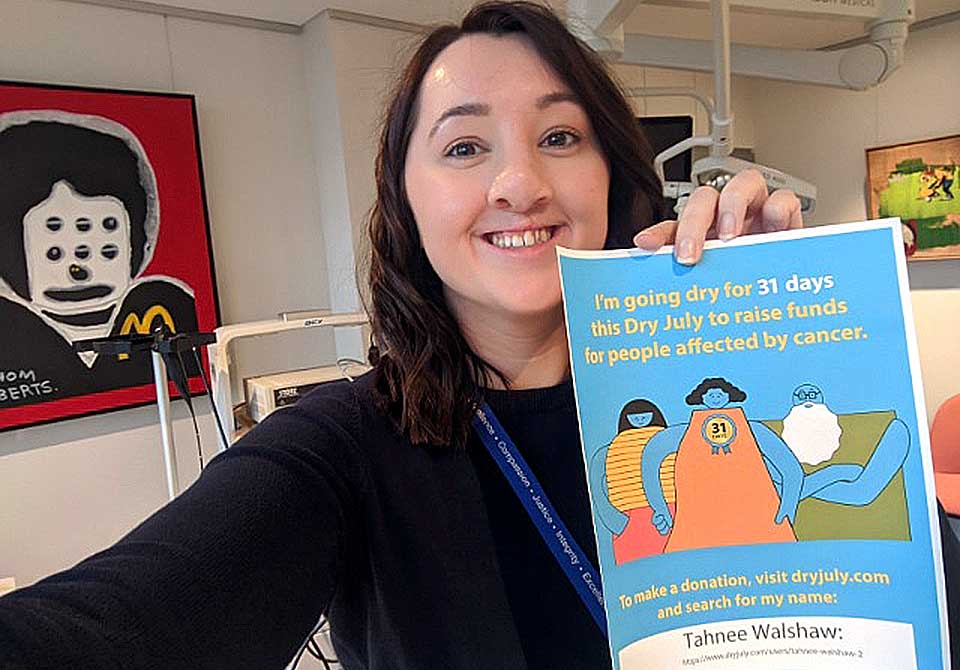
Tahnee, my fantastic Practice Manager, is doing Dry July this year. Dry July is a fundraiser that encourages Australians to go alcohol-free in July to raise funds for people affected by cancer. Tahnee is a braver soul than me and I want to support her to go dry this July. Realising I do not want to go dry this July myself has forced me to reflect on my own alcohol consumption, the relationship between alcohol and cancer, and the implications of alcohol withdrawal for Head and Neck surgical patients.
Alcohol and Head and Neck Cancer
I don’t want this to be another online article lecturing about the cause and effect relationship between alcohol and cancer. Not all Head and Neck cancers are related to smoking or drinking. But many are. For those of you who do smoke and drink, giving up smoking is by far the single most important thing you can do to improve your short term and long term treatment outcomes.
How many drinks do you have a week?
As a doctor I ask this question every time I see a new patient. I’ll let you in on a secret. I usually add a third to the amount you tell me. Not because I think you’re a liar, or a bad person, but because it helps to balance how much you like to think you drink on a good day with the amount you actually drink on a bad day. Mind you, there are also plenty of patients who are brutally and impressively honest. If you drink whiskey for breakfast and you tell me about it then your honesty goes a long way towards building trust in our doctor-patient relationship. Even more importantly, if you require surgery this information helps the team of doctors and nurses looking after you to better manage your care and make you more comfortable.
Surgical patients and alcohol withdrawal
Often the time between a Head and Neck cancer diagnosis and commencement of treatment is very short. Too short for patients to gradually ease their tobacco or alcohol consumption in order to avoid withdrawal symptoms in hospital. This situation does not just apply to Head and Neck cancer patients. There are plenty of in-hospital patients who experience alcohol withdrawal. Usually they are unaware that withdrawal is exacerbating their anxiety and agitation. But experienced nurses on the wards do recognise the symptoms. That is why if you’re a patient in the private hospital, and you’re eating and drinking a normal diet, a nurse might suggest you have a glass of wine with dinner. Unfortunately, this option does not exist for the majority of Head and Neck cancer surgical patients who are unable to swallow after surgery. In that instance, if we think it is required, we may use medication to ease your symptoms.
What are the signs of alcohol withdrawal?
The typical signs of alcohol withdrawal include sweating, anxiety, depression and insomnia. The severity of symptoms, however, changes depending upon how much you drink, also known as your level of dependency. If you let us know you have an alcohol dependency before you are admitted to hospital as a surgical patient, or if we suspect it, we will commence a formal Alcohol Withdrawal Scale (AWS) when you exit surgical recovery or intensive care (ICU) and enter the ward. This is a monitoring rather than a diagnostic tool but it helps the team of people engaged in your care keep an eye on your condition and intervene with medication if required.
When do symptoms start to appear?
Patients with alcohol withdrawal typically start to show symptoms two to three days after surgery. Behaviour is usually the giveaway. If patients become unusually anxious or agitated then we know something is going on. There are seven criteria we use to monitor, rank and manage your severity of withdrawal. These include;
- Perspiration
- Tremor
- Anxiety
- Agitation
- Temperature
- Hallucinations
- Orientation
A couple of times each year I have patients who experience severe alcohol withdrawal. Unfortunately, this can result in physical and verbal abuse of nursing staff, a situation which we would all prefer to avoid.
Carers can also feel the impact
Carers of cancer patients travel their own cancer journey. Sometimes this journey involves supporting a loved one as they go through withdrawal while receiving treatment, sometimes it involves going through deliberate, sympathetic withdrawal as an act of support, sometimes it is inadvertent withdrawal due to a change of routine or living conditions. The good news is that withdrawal symptoms should improve, but please make sure to seek support, even if you think you’re doing fine without it.
Honesty is the best policy
So, this Dry July, in addition to donating to Tahnee’s campaign, I’m going to ask you to also join me in reflecting upon your personal alcohol consumption. I won’t be asking how much you drink unless you’re a patient. But being honest, whether it is with yourself, your loved ones, or your doctor, can do a lot of good.