Introducing Orsi Kokai
I invited physiotherapist Orsi Kokai to explain the multiple ways in which specialist physiotherapists can help reduce and manage long term side effects associated with the treatment of head and neck cancers.
ORSI KOKAI: Thank you Richard. Every day in my practice I see patients with side effects from different types of cancer treatment. Some side effects are related to surgery, others are related to radiotherapy and chemotherapy. As a general rule, the earlier I see patients the more I can do to help them. In this article I describe the physical side effects I treat and the symptoms to look out for, the way I work with patients, the importance of treatment plans, plus the two key stages in head and neck cancer treatment when patients should be screened by head and neck cancer clinicians for referral to a specialist physiotherapist.
Side effects related to surgery
The major side effect I manage in head and neck surgical patients is injury to the accessory nerve resulting in temporary weakness of the shoulder. Unfortunately this can develop into long term shoulder dysfunction and long term pain. The accessory nerve controls the trapezius muscle. The trapezius is the big muscle which helps elevate your shoulder. Patients most at risk include those who undergo surgery to remove lymph nodes from the neck known as a neck dissection. In some patients this side effect appears immediately after surgery. In other patients it appears further down the track. In many cases neck mobility can be restricted which may impact on everyday activities such as driving.
A specialist head and neck physiotherapist  can help manage this side effect in a number of different ways. This ranges from manual techniques to relieve tension and encourage correct muscle use to prescribing exercises to gradually strengthen weakened muscles. Advanced understanding of the anatomy of the head and neck is part of being a specialised head and neck physiotherapist. I am fortunate to have observed Richard operate in theatre and seen for myself how surgery may cause the side effects I treat.
Depending on the extent of the surgical intervention, side effects can include pain, altered sensations, reduced motor function of the neck, jaw or shoulder, and decreased strength. These symptoms are often the result of natural scarring and fibrosis. Scarring and fibrosis may make the skin of the neck feel thickened and stiff and include a sensation of pressure. Stiffness may also be the result of swelling and immobility. Manual treatment can be especially helpful for patients to help reduce these side effects.
It can be very difficult for patients to know whether or not the sensations they feel around a healing neck are normal. It is important to discuss these symptoms with your surgeon, radiation or medical oncologist in order to distinguish between the body’s normal healing process and more severe physical side effects which may benefit from specialist physiotherapy treatment.
Side effects related to radiotherapy and chemotherapy
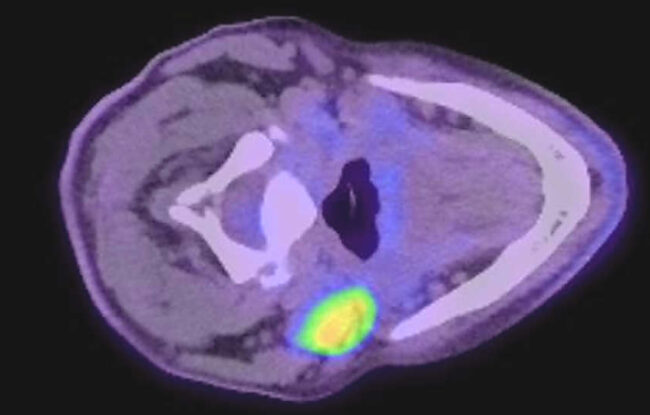
The side effects of radiation treatment tend to be localised to the area that is being treated and can impact on skin integrity, speech, swallowing and movement of the neck or jaw. The side effects of radiotherapy are always exacerbated if chemotherapy is also involved. This is because the chemotherapy increases the local toxicity of the radiotherapy. The major side effect I manage for patients who have been treated with radiotherapy is lymphoedema. Lymphoedema, sometimes referred to as oedema, is the accumulation of fluid in the tissue spaces due to damage of the lymphatic system. This results in swelling which can be mild and reversible or severe and permanent.
Head and Neck Lymphoedema (HNL) can occur on both the inside and the outside of the neck. Internal HNL can affect vital functions like breathing, speech, swallowing and chewing, whereas external HNL may lead to decreased range of motion in the neck and shoulders and greatly impact a patient’s appearance. External lymphedema, when severe, may lead to issues with body image and social avoidance. The most frequently involved external anatomical sites are the submental region, where a boxer would try to land an uppercut on the chin, and the neck. External lymphoedema presents as a soft, painless lump which may become inflamed or uncomfortable. The size of the lump can change from day to day and from morning to evening. Patients with internal lymphoedema commonly describe tightness in the throat and difficulty swallowing.
Lymphoedema symptoms most commonly appear towards the end of radiotherapy or in a few months after the completion of radiotherapy. As per shoulder weakness, it is best to discuss these symptoms with your surgeon, radiation or medical oncologist so you can benchmark which symptoms may be temporarily related to cancer treatment and which symptoms indicate a more serious side effect which would benefit from treatment by a head and neck physiotherapist.
Trismus, or difficulty opening the mouth, is another side effect which physiotherapists can help manage. Trismus is caused by swelling of muscles which open the mouth. Sometimes trismus is directly caused by the position of a cancer, in other patients it is a side effect of cancer treatment. It is most common among patients who are treated with radiotherapy.
Radiotherapy can also cause long term fibrosis in the skin and underlying tissues. Patients with fibrosis of the neck who are referred to a specialist physiotherapist report that physiotherapy and massage help reduce discomfort and pain and help to restore mobility.
Treatment team includes the patient
The management of side effects after treatment for head and neck cancer requires team work. To ensure best possible outcomes it is important to include the patient in the team. This starts with education. Part of my job is to help patients understand the reason behind his or her limitations. Explaining what happens when the nerves are damaged, why muscles are weakened, or why limitations of movement occur, is an important part of the management process. Describing the function of the lymphatic system and why swelling happens when the lymph nodes are removed, or the lymphatic pathways are compromised, ensures that the patient understands the process and is likely to be proactively involved in the management. The physical side effects of cancer treatment very often have an impact on quality of life. The role of a specialist physiotherapists is to manage physical limitations. We often refer to other health professionals when side effects are identified which don’t fall into our scope of practice.
Importance of treatment plans
Once the limitations are correctly identified and patient education has taken place, the next step is to put together a treatment plan focusing on the patient’s individual goals. Treatment usually consists of a range of hands-on physiotherapy techniques to assist movement, decrease tightness or swelling. It involves individually tailored exercises to prevent or manage physical de-conditioning or to improve strength and includes the prescription of self-management strategies to provide continuity. The severity of symptoms and the timing of the intervention determines the frequency of visits. My ‘mantra’ to the patient is: The more you do, the less you will need me. Some of the side effects however require ongoing monitoring or maintenance. If for example the swelling of the neck is not responding to manual techniques only, it is often necessary to apply compression to the affected area. This needs to be monitored and adjusted as symptoms are changing.
When to seek a referral to a specialist physiotherapist
Patients who are concerned about possible side effects from head and neck cancer treatment should discuss them with their surgeon, radiation oncologist, cancer care coordinator, cancer nurse, nurse practitioner or GP (general practitioner). I know that the intense and grueling nature of cancer treatment can make it hard to involve a physiotherapist early in patient care but the sooner we are brought in to help manage side effects the better we can help prevent temporary side effects from becoming long term or permanent problems. There are two key stages in the head and neck cancer treatment Âprocess when clinicians should consider referring a patient to a specialist head and neck cancer physiotherapist:
- After surgery – if a patient has limited function of the neck or the shoulder Âas a result of surgery, they can be referred to a physiotherapist for hands on treatment and prescription of specific exercises. This assessment is best made Âbefore the commencement of any radiotherapy.
- After radiotherapy treatment is completed – radiation may further limit neck or shoulder function. Patients often experience increased tightness or swelling during or after completion of radiotherapy. Assessment by a specialist physiotherapist is recommended to identify existing symptoms and to prevent long-term complications. Â Delaying referral Âmay lower the benefits of physiotherapy treatment.
In conclusion
A head and neck specialist physiotherapist can help assess, manage and reduce physical side effects of head and neck cancer treatment. Not all physical side effects develop during or immediately after cancer treatment and may emerge further down the track. This means that I may see the same patient for different side effects at different stages of their cancer journey. A specialised physiotherapist not only understands which intervention can be applied without causing injury to the treatment site but also will be alert to the possible development of secondary physical side effects. Therefore, it is important to refer patients to physiotherapists who are experienced in treating head and neck cancer patients.
You can make an appointment with Orsi at The Kinghorn Cancer Centre Wellness Centre in Darlinghurst or at Oncology Recovery Services Inc (ORSI) in Kingsford. Orsi also runs free three monthly support groups for people affected by head and neck cancer. To find out more visit her website or email ok.physio@gmail.com