The management of idiopathic subglottic stenosis (ISGS) continues to evolve. Patients are often placed on medications to decrease the inflammation and consequent scarring that characterises the disease process. Prednisone (synthetic corticosteroid) may be used in both short and long term management. Due to side effects, we often use steroid sparing drugs.
Surgery, however, remains the primary treatment. All patients require an initial endoscopic assessment and treatment under anaesthetic. Many patients will require this endoscopic treatment to be repeated over their lifetime.

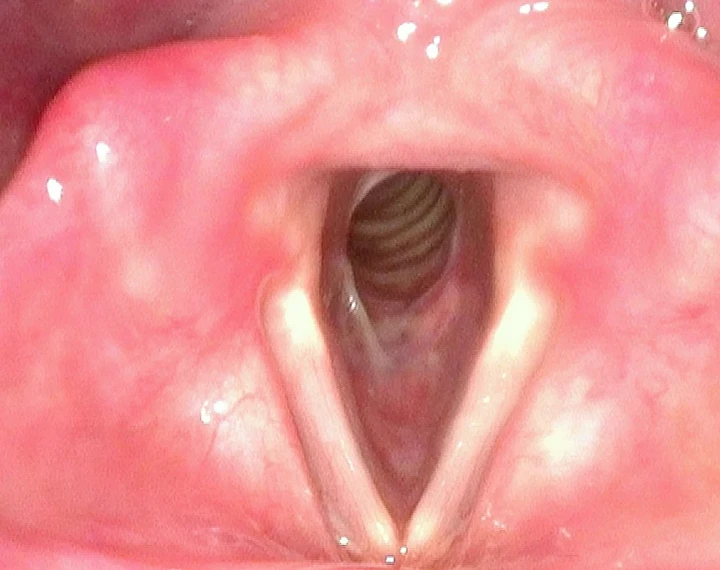
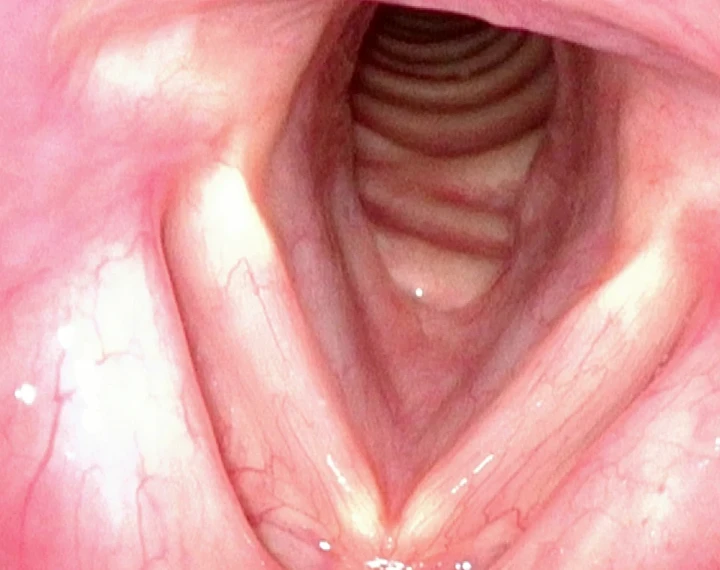
Image Sequence
- After 5 years of multiple endoscopic treatments the patient was referred with acute airway distress. The subglottic airway was 4mm (normal 12-20mm).
- Following endoscopic treatment the airway was much improved. The patient required repeated procedures and lived in a rural location.
- The patient proceeded with a cricotracheal resection and this image is 18 months post surgery
Diagnosis
ISGS is difficult to diagnose and is quite often mistaken for other common respiratory diseases such as asthma. Regularly I will treat patients whose diagnosis has been delayed. This can be a real problem because these patients have airway obstruction which continues to evolve and is not reversible with drugs. Consequently, subglottic stenosis can be a threat to life.
Patients should be referred to an ENT surgeon who will perform a flexible examination of the larynx in the office and make the diagnosis. This is much simpler for patients in metropolitan areas, whereas those who live in the regions will generally face a shortage of specialists.
Initial management is aimed at restoring the airway and performing a biopsy. During my training in the early 1990’s quite a few patients ended up with a tracheostomy. Nowadays repeated endoscopic management is the standard treatment. This can put a significant psychological, travel and financial burden on patients, particularly if they require frequent treatment.
Endoscopic Management
This procedure is performed under general anaesthesia. It requires close teamwork between the surgeon and anaesthetist who share the airway together. There are many different approaches to managing the stenosis. I tend to utilise a combination of laser, steroid injection and balloon dilation depending on the case.
Each patient is different, some require infrequent endoscopic treatment, maybe once a year or less. These are the lucky few. Most will require repeated treatments, in some cases up to four times per year.
ISGS can start at any time during adulthood, even during pregnancy. Patients may be facing endoscopic treatment for the rest of their lives. Understandably, this has a psychological impact on patients, creating anxiety and affecting other family members. It also creates a significant financial burden, due to multiple appointments, surgeries, travel and accommodation to manage what is a chronic disease process.
Cricotracheal Resection
Cricotracheal resection is an open surgical approach aimed at providing long-term cure. The aim is to remove the soft tissue inflammation and scarring within the subglottis, including any involved trachea. In ISGS the cricoid cartilage is not involved, the problem is within the lining. The area is reconstructed using normal trachea and mucosa.
This is a complex operation which takes around four hours to perform. At the end of the procedure the breathing tube (endotracheal) is removed in the operating room and the patient spends the night in the intensive care unit. The hospital stay that follows lasts a week as close observation is required. Whilst no surgical procedure is entirely without risk complications are rare.
Open surgery is naturally a confronting option for most patients. To assist patients in making an informed choice about undergoing a cricotracheal resection I will commonly put them in touch with patients who have had the procedure.


