Our patient had sought treatment in Thailand where he presented with a neck lump. Commonly, as was the case with our patient, these lumps are lymph nodes into which cells of a squamous cell carcinoma (SCC) have spread. His Thai medical team had confirmed this through biopsy and went on to surgically remove this positive lymph node.
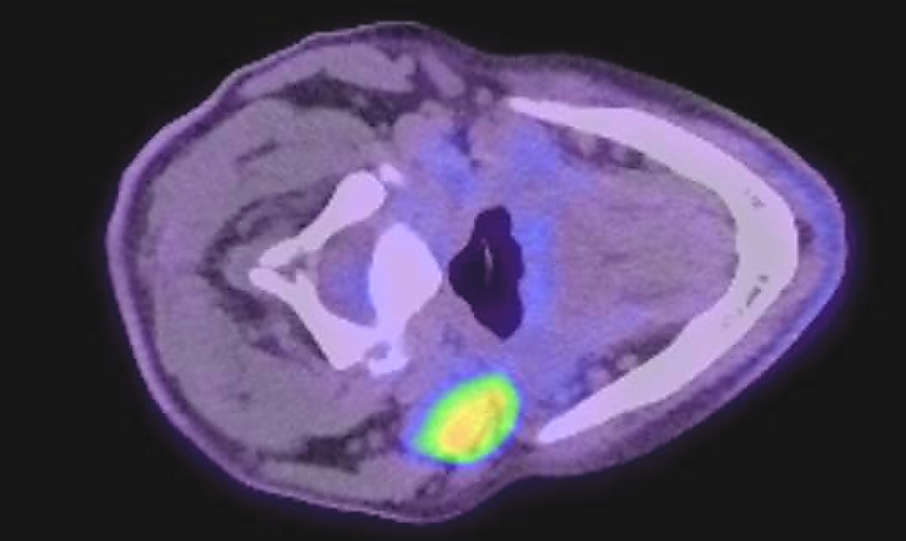
When he first presented at our Clinic here in Sydney for a second opinion he did not present with any clear symptoms of a head and neck cancer. Neck lumps unfortunately can often be the only obvious evidence of an underlying and serious malignancy. His prior history meant I could rule out lymphoma, so we would need to rely on diagnostic testing to assist in determining the primary site of origin. These tests included PET and diagnostic CT scanning and fine needle aspiration biopsy.
The tests confirmed that the patient had metastatic cancer in multiple lymph nodes of the left neck. Immunohistochemical testing detected the presence of the p16 protein within the cells of the biopsied lymph nodes. The likelihood of this being driven by HPV is high, and further testing confirmed our patient had HPV-mediated 16+cancer.
At this stage we still had an unknown primary setting. That said, it is well understood that HPV driven head and neck squamous cell carcinomas (HNSCC) are mostly found in the oropharynx, specifically arising from tonsil tissue which includes the palatine and lingual tonsils. Certainly, this aligns with my experience of increasing numbers of cases of HPV related HNSCC.
The patient then attended a St Vincent’s Head and Neck Multidisciplinary Team (MDT) meeting (this meeting is held weekly). Given the patient history and pathology we decided on transoral robotic surgery (TORS) to resect the left palatine and left lingual tonsils with accompanying surgical pathology. We decided against removing the left lymph nodes (neck dissection) in favour of adjuvant radiotherapy and chemotherapy.
TORS surgery is minimally invasive surgery, which brings a number of advantages, not the least of which is less trauma to the body and quicker healing. Moreover, surgery as a primary treatment would allow us to avoid extensive radiotherapy and chemotherapy. In particular, this approach would allow us to de-intensify the radiotherapy by targeting only the lymph nodes, thus reducing the fields and dose. In this case radiotherapy was not given to the throat which reduces long term complications.
The robotic surgery went to plan. As predicted, squamous cell cancer was found in both tonsils. Our journey to find the primary was over. For this patient the primary was in the left lingual tonsil. The tumour was relatively small at 9mm x 7mm x 4mm, well under the T1 staging (which specifies less than or equal to 2cm in the greatest dimension). Primaries of this size or smaller are difficult to detect even with modern imaging tests.
Cancer in the left neck lymph nodes was treated post-operatively with chemoradiotherapy. After a three month period of adjuvant treatment our patient was cancer free and has remained so. He returned to Vietnam and continues to visit us in Sydney for his scheduled monitoring over five years. This case was considered a success, and underlines the importance of finding the primary and choosing minimally invasive surgery as the primary treatment.