We have just completed the second annual St Vincent’s Head and Neck Dissection course.
In Australia, Otolaryngology – Head and Neck Surgery trainees must complete four accredited dissection courses during an average of five years of training. These include two temporal bone courses, a sinus course, and a head and neck course. The St Vincent’s Head and Neck Dissection Course differentiates itself from other courses on offer in a number of ways, including exposing trainees and observers to rarer surgical techniques such as laryngeal framework surgery and partial laryngeal cancer surgery. These procedures are important because they maximise quality of life for patients after cancer treatment. This is very different to the approach I was taught twenty-five years ago when the focus was eradicating cancer at any cost.
The role of dissection courses in surgical training
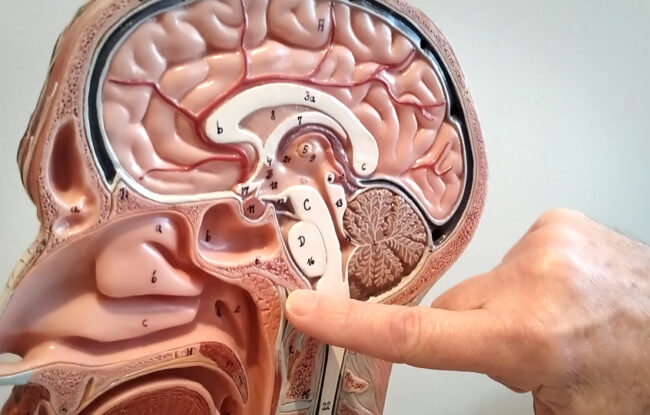
I started the St Vincent’s Head and Neck Dissection course with my colleagues in 2018 to ensure that surgical trainees could develop an understanding of some of the complex procedures that head and neck surgeons regularly perform. During training the majority of junior Otolaryngology – Head and Neck surgeons in Australia and New Zealand may only observe these procedures and never have the opportunity to perform them. A cadaver dissection course gives them the opportunity to complete the procedure from start to finish away from the pressures of the operating room. They develop a deeper understanding of the anatomy and learn how to access different areas of the head and neck.
Dissection courses are an essential part of surgical training for all surgical trainees. The teaching of anatomy in medical schools has been a topic of debate for many years. Cadaver dissection is the gold standard of anatomy training and dates back to the ancient Greeks, but the prohibitive costs of cadaver dissection and technological advances, such as computer simulators, online learning platforms, and 3D printed anatomical kits, has resulted in many Australian medical students rarely encountering a cadaver.
There are two types of enrolment in the St Vincent’s Head and Neck Dissection Course, as a dissector or an observer. Our 2019 participants included consultant surgeons, surgical trainees, nurses, specialist physiotherapists and medical students.
How our course is different
At the St Vincent’s Head and Neck Dissection course we do several things differently to similar courses on offer around Australia;
- Operative procedures and dissections are filmed ahead of time. During the course we play the videos on the eight overhead monitors while the instructor describes what’s happening. This allows the instructor to fast forward through the non critical stages of the procedure, translating into less time demonstrating and more time dissecting.
- Participants enrolled as dissectors get to take the videos home on USB for further review.
- We focus on advanced surgical techniques which are in decline due to the increase in minimally invasive surgery (MIS).
- Our cadavers have the upper shoulder and thorax intact.

Dissections and procedures are recorded ahead of the course and played on overhead monitors. Instructors can fast forward through non critical stages, allowing more time for hands on dissection.
Surgical procedures demonstrated
As a supervising consultant surgeon, retired RACS Board Examiner, and retired National Board Chair of Otolaryngology Head and Neck Surgical training, I noticed several years ago that today’s surgical trainees are not being exposed to the same volume of complex head and neck surgical procedures as I did during my training. In particular I realised that many trainees are admitted to the Royal Australasian College of Surgeons (RACS) having been exposed to very few examples of;
- open partial laryngeal surgery
- laryngeal framework surgery and arytenoid procedures
- complex or extended neck dissection involving selection of the lymph nodes
- total maxillectomy
This decline is in part due to an increase in minimally invasive surgery (MIS) techniques, but I also know from my numerous conversations with registrars that it is also because there are fewer consultant surgeons who are capable of performing some of the rarer complex procedures such as partial laryngectomy. Demand for these procedures may have decreased but there is still a need to maintain this specialist knowledge and expertise, especially when it comes to maximising patient quality of life after cancer treatment. Partial laryngeal surgery is a particular favourite of mine. I find it enormously rewarding to be able to simultaneously treat a patient’s laryngeal cancer and preserve their ability to speak.
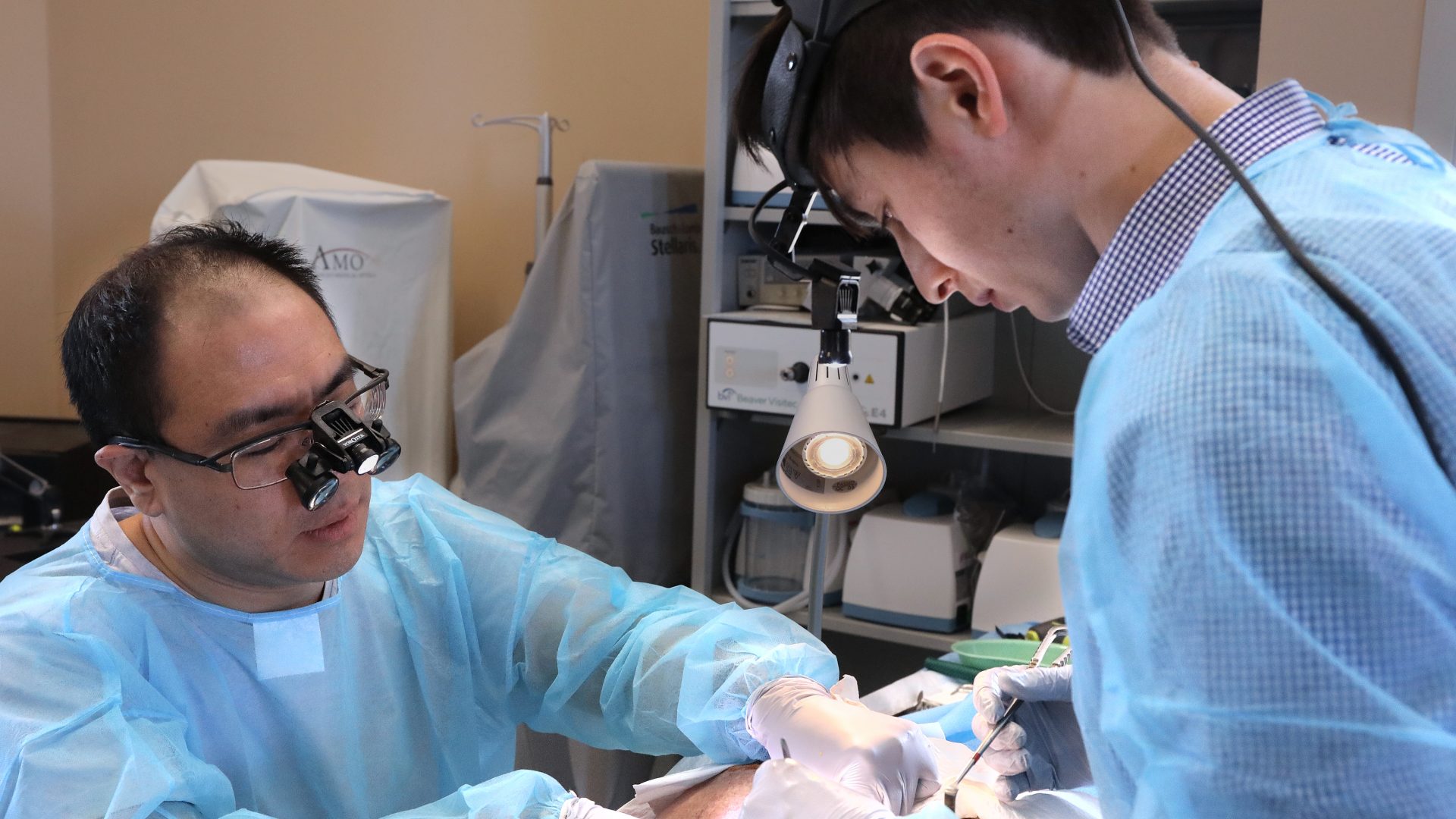
Dissectors hard at work. Our cadavers include the thorax and shoulders which is important for teaching neck dissection.
Championing Head and Neck surgery within Ear, Nose and Throat
The Royal Australasian College of Surgeons consolidated training of Head and Neck Surgery within the specialty of Otolaryngology (Ear, Nose and Throat) in 1998. Â As a teaching member of my specialty with the responsibility of passing on this particular surgical knowledge I decided that NSW needed a Head and Neck Dissection Course run by an Otolaryngology – Head and Neck Surgery service. We do not run the Head and Neck Dissection Course on the St Vincent’s Hospital campus because there is an excellent Research and Training Laboratory three kilometres down the road at Sydney Hospital. The laboratory is specifically designed for teaching and has eight dissection stations and eight high resolution monitors which can accommodate our relatively large cadavers. Furthermore, the relationship between Ear, Nose and Throat and Sydney Hospital goes back many decades. It is a fantastic venue which brings back many fond memories for NSW surgeons.

The Sydney Hospital Research and Training Laboratory is ideal for our purposes. It allows for eight dissection stations and two dissectors per cadaver with plenty of room for observers and instructors.
A team effort
I am proud that the faculty of our course included ten surgeons representing five different hospitals from Sydney, Newcastle, Melbourne, Adelaide and Perth. Thank you to Assoc Prof Ron Bova, Dr Daron Cope, Dr Julia Crawford, Dr Ben Dixon, Dr Andrew Foreman, Dr Georgina Harris, Dr Brett Leavers, Dr Richard Lewis, and Dr Catherine Meller. I particularly want to thank Ben, Andrew and Richard for traveling from interstate. Your input was invaluable
I also want to thank Dr Julia Crawford and Dr Brett Leavers for co-convening the meeting, Julia’s PA Veronica for ‘making things happen’, and the fantastic Research and Training Laboratory team at Sydney Hospital. And thank you to our gold sponsors Device Technologies, our silver sponsor Lumenis, and our in-kind sponsors Atos Medical, St Vincent’s Private Hospital, and Zeiss Medical Technology. Convening and presenting at the dissection course reminds me how much I love teaching. We had a fantastic weekend thanks to the commitment of our presenters and the curiosity of our participants. Â I look forward to doing it all again next year.